Items filtered by date: May 2024
When Surgery Is Needed for Heel Spurs
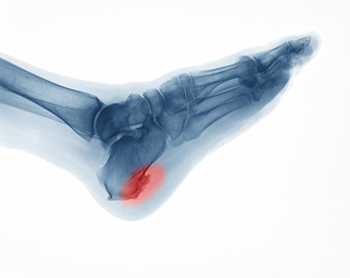
When conservative treatments prove ineffective in easing the discomfort, inflammation, and swelling associated with heel spurs, surgery emerges as a viable solution. These outgrowths on the heel bone, medically termed calcaneal spurs, can cause significant pain and impede mobility. The decision to pursue surgery hinges not solely on the size or presence of the spur, but rather on the persistence of pain resistant to treatment. Podiatrists typically advocate for surgery when symptoms persist despite six months of non-surgical interventions. Two primary approaches exist for heel spur surgery, which are known as open surgery and endoscopic surgery. Open surgery entails larger incisions and is generally employed to excise entire spurs. Endoscopic surgery employs smaller incisions, fostering quicker recovery and fewer complications. The surgical procedure may vary depending on the spur's location, whether it is inferior or posterior. Inferior heel spurs often coexist with plantar fasciitis and are addressed through plantar fasciotomy. Posterior heel spurs near the Achilles tendon may necessitate more intricate procedures, especially if the spur is deeply embedded within the Achilles tendon. While heel spur surgery has a high success rate, it also carries risks of nerve injury, foot instability, and acquired flat feet. If you are in pain from a heel spur, it is suggested that you consult a podiatrist who can determine what the best course of treatment is for you.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Passaic, NJ . We offer the latest in diagnostic and treatment technology to meet your needs.
We Can Treat Your Foot or Ankle Pain
Three Types of Corns on the Feet

Corns are identified as patches of thickened skin and are a common foot problem that can cause discomfort and pain if left untreated. Understanding different types of corns can help in effectively managing and preventing them. Hard corns, the most prevalent type, typically develop on the tops and sides of toes or weight-bearing areas of the foot. These corns are compact and dense, often caused by friction or pressure from wearing ill-fitting shoes or repetitive motion. Conversely, soft corns tend to form between toes where sweat and moisture accumulate. These corns are softer in texture and can be more painful due to increased moisture levels. Finally, seed corns are tiny, discrete corns that often appear on the bottom of the foot. They are generally painless but can cause discomfort when walking. If you have a corn on your foot, it is suggested that you consult a podiatrist who can identify which type it is, and offer you correct treatment solutions.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Custom Orthotics Seasonal - Any Season

Rain or shine, snow or sleet, Custom Orthotics have your feet covered! As the seasons change, ensure your steps remain comfortable and supported. Custom Orthotics adapt to your footwear, from summer sandals to winter boots, providing consistent relief and alignment. Don't let the changing weather dictate your foot comfort. Step confidently year-round and experience the difference with Custom Orthotics. Call today for more information.
Can Bunions Become Worse?

A bunion, medically termed hallux valgus, is a bony bump that forms at the base of the big toe. This condition develops when the big toe pushes against the adjacent toe, causing the joint to protrude outward. Bunions can result from various factors, including genetics, wearing tight or ill-fitting shoes, and foot injuries. Individuals with certain foot types, such as flat feet or low arches, are more prone to developing bunions. Additionally, occupations or activities that involve repetitive stress on the feet can increase the risk. Bunions are a relatively common foot ailment, affecting millions of people worldwide, with women being more susceptible than men as a result of wearing high heels or narrow shoes that can worsen the condition. While bunions may initially cause mild discomfort, they can progressively worsen, leading to pain, inflammation, and difficulty walking. A bunion can be uncomfortable, and a podiatrist can offer you effective relief strategies. If you have this condition, it is suggested that you consult this type of doctor who can offer appropriate treatment methods.
If you are suffering from bunion pain, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Custom Foot Orthotic Assessment

Foot orthotic assessment, particularly for custom orthotics, is an important step in addressing various foot conditions and promoting optimal foot health. Custom orthotics may be necessary to correct biomechanical abnormalities, provide support, and alleviate pain associated with conditions like plantar fasciitis, flat feet, or arthritis. When assessing for custom orthotics, podiatrists consider important joints in the foot, such as the subtalar, midtarsal, and metatarsophalangeal joints. These joints play a significant role in foot function and alignment, making them key areas for orthotic intervention. The assessment process involves an examination of foot structure, gait analysis, and identification of specific areas of concern or dysfunction. Podiatrists work closely with patients to develop personalized orthotic solutions tailored to their individual needs and conditions. If you are experiencing foot pain or discomfort, a professional assessment from a podiatrist is suggested to determine if custom orthotics are the right treatment option for you.
Experience a transformative solution to heel pain and foot pain through the personalized benefits of custom orthotics and shoe inserts. If you’re grappling with the persistent agony of plantar fasciitis, these customized inserts are designed to alleviate the strain on the plantar fascia, providing targeted relief. Engineered to adapt to your unique foot anatomy, custom orthotics tackle not only plantar fasciitis but also general foot and heel pain, offering unparalleled support and comfort. Don’t let every step be a reminder of discomfort; step into a world of tailored well-being. Say farewell to the limitations imposed by heel pain and embrace the freedom of pain-free mobility. Invest in your foot health and redefine your daily stride with the transformative power of custom orthotics and shoe inserts, ensuring each step is a step towards lasting comfort.
If you have any questions please contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Peripheral Neuropathy and Its Impact on the Feet

Peripheral neuropathy is a condition characterized by damage to the nerves outside the brain and spinal cord. It often results in such symptoms as numbness, tingling, and weakness in the extremities. When it affects the feet, peripheral neuropathy can negatively impact mobility and quality of life. The nerves responsible for sensation and motor function in the feet may become impaired, leading to loss of sensation, burning pain, or hypersensitivity. These symptoms can make it challenging to walk or perform daily activities. Additionally, peripheral neuropathy can cause complications, such as foot ulcers and infections, particularly in individuals with diabetes. Regular foot care and monitoring are essential for preventing serious complications. Managing underlying conditions and adopting lifestyle changes, such as maintaining optimal blood sugar levels and wearing supportive footwear, can help alleviate symptoms and improve overall foot health for individuals with peripheral neuropathy. If you have this condition and your feet are affected, it is suggested that you are under the care of a podiatrist who can help you manage peripheral neuropathy.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.