Rheumatoid Arthritis and the Feet

Rheumatoid arthritis, or RA, is an autoimmune disease that causes chronic inflammation in the joints, including those in the feet and ankles. It can lead to pain, swelling, stiffness, and deformities such as hammertoes, bunions, and collapsed arches. Over time, the cartilage in the foot joints may erode, causing joint damage, reduced mobility, and difficulty walking. The constant inflammation can also affect soft tissues, leading to tendon damage and further deformities. A podiatrist plays a vital role in managing foot symptoms associated with RA. They can provide treatments like custom orthotics to support foot alignment, relieve pressure, and improve comfort. They can also prescribe anti-inflammatory medications or provide corticosteroid injections to manage pain. In severe cases, surgery may be necessary to correct deformities. If you have rheumatoid arthritis, it is suggested that you visit a podiatrist regularly for treatment to prevent further joint damage and maintain mobility.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.
What Is Peripheral Neuropathy and How Does it Feel?

Peripheral neuropathy is a condition affecting the peripheral nervous system, which consists of the nerves outside the brain and spinal cord. This system relays information between the central nervous system and the rest of the body, controlling sensations, movements, and autonomic functions. Peripheral neuropathy occurs when these nerves are damaged, leading to symptoms like tingling, numbness, pain, and weakness, often in the hands and feet. It can result from diabetes, infections, autoimmune diseases, toxins, or even trauma. Small fiber neuropathy specifically affects the small sensory fibers responsible for pain and temperature regulation. This type of neuropathy can cause burning or stabbing pain, tingling, or sensitivity to temperature. It often occurs in conditions like diabetes, but it can also be caused by other factors such as genetic disorders or autoimmune diseases. If you are feeling symptoms of peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist for an early diagnosis and management to prevent worsening of symptoms and nerve damage.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
The Impact of Flip-Flops on Foot Biomechanics and Gait

Flip-flops, while popular for their convenience and comfort, can negatively affect foot biomechanics and gait. These minimalistic shoes offer limited support and cushioning, leading to poor alignment of the foot and increased stress on the muscles and joints. The lack of arch support and cushioning can cause abnormal gait patterns, such as overpronation or supination, which may result in foot pain or discomfort. Additionally, the loose fit of flip-flops requires constant gripping with the toes to keep them on, which can strain the foot muscles and contribute to imbalance. Over time, frequent use of flip-flops may worsen existing foot problems or lead to new issues such as plantar fasciitis or metatarsalgia. If you have developed one or more foot conditions from wearing flip-flops, it is suggested that you consult a podiatrist for effective treatment.
Flip-flops are not always the best choice of footwear. If you have any concerns about your feet or ankles, contact Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
When the weather starts warming up, people enjoy wearing flip-flops. Flip-flops are comfortable, stylish, and easy to slip on and off; they're perfect for any summer beach goer. However, these shoes can cause harm to the feet.
How Can Flip-Flops Affect Me Long-Term?
- Ankle problems
- Hip problems
- Lower back problems
- Pain in the balls of the feet
- Problems with foot arches
- Changes in the way you walk
Are There Injuries Associated with Flip-Flops?
Yes. Since flip-flops are relatively weak and do not provide the same amount of support as sneakers, people who wear flip-flops regularly are more susceptible to injuries. On top of that, the open nature of the shoe makes your feet more prone to other problems, such as cuts and even infections. Common injuries and ailments include:
- Sprained ankles
- Blisters
- Infections
- Cuts and Scrapes
I like Wearing Flip-Flops. Are There Safe Alternatives?
When buying flip-flops, try to find ones that have sturdy soles and that are made of high-quality materials that will support for your feet. These flip-flops will cost more but will also last longer as a result.
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flip Flops and Your Feet
When the weather heats up, you may want to start wearing flip-flops. However, it has been proven that these are not the ideal shoes in terms of preserving the health of your feet.
Flip flops are known to expose your feet to different types of bacteria and fungal infections. When you wear your flip flops in public, you are exposing them to staphylococcus which is a skin-irritating bacterium. Athlete’s foot is also highly contagious and can be spread when you walk around nearly-barefoot.
Another harmful effect of wearing flip-flops is that they develop blisters on the feet. This is because the thin strap rubs against the skin with each step taken. Unfortunately, when blisters pop, they cause you to be more vulnerable to pathogens you pick up by having your feet exposed.
These shoes may also cause “shooting pains”. If you have flat feet, you need arch support to keep your knees, hips, and back in alignment. If you wear flat shoes, your joints are forced to compensate which can cause injuries throughout the body.
If you constantly wear flip-flops, you should avoid doing so as they can lead to many problems for your feet. If you are experiencing any of these foot issues, you should seek help from a podiatrist right away.
Bypass Bunion Surgery with Custom Orthotics

Considering bunion surgery? Think again. Custom Orthotics offer a non-surgical approach to reduce pain and restore foot function. Customized to your foot's structure, they realign and redistribute pressure, alleviating bunion discomfort. Experience the freedom of movement without the downtime and risks of surgery. Contact our office to make an appointment.
Facts About the Achilles Tendon and Potential Injuries
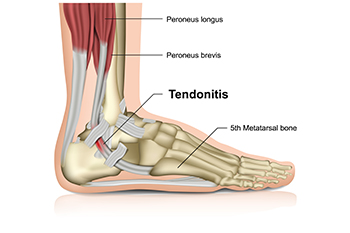
The Achilles tendon, the largest tendon in the body, connects the calf muscles to the heel bone, playing a vital role in walking, running, and jumping by facilitating the movement of the foot. Achilles tendon injuries often result from overuse, excessive strain, or sudden increases in physical activity. Causes include repetitive stress from activities like running or jumping, improper footwear, or muscle imbalances. People prone to these injuries include athletes, especially those involved in sports requiring quick changes in direction, and anyone who suddenly intensifies their exercise routines without proper conditioning. Other risk factors include age-related tendon degeneration and pre-existing conditions like diabetes or arthritis. Achilles tendon injuries can cause severe pain and discomfort. If you have sustained this type of injury, it is suggested that you promptly consult a podiatrist who can effectively treat and manage this condition.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.